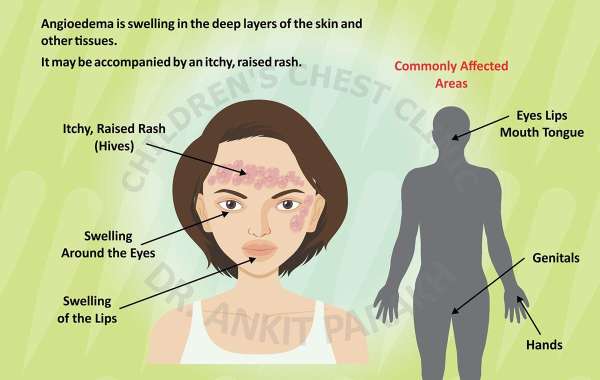
Angioedema is a medical condition characterized by sudden, localized swelling beneath the skin, often affecting areas like the face, lips, throat, or extremities. It can be triggered by allergic reactions, medications, hereditary factors, or other underlying causes. The swelling can be uncomfortable, disfiguring, and, in severe cases, life-threatening if it obstructs the airway. Effective treatment depends on the underlying cause, severity, and frequency of episodes. This article explores the best treatments for angioedema, incorporating medical interventions, lifestyle adjustments, and preventive strategies, while addressing the role of medications like those supplied by a Cephalexin supplier in specific contexts.
Understanding Angioedema
Angioedema results from the release of histamine and other chemicals that cause blood vessels to leak fluid into surrounding tissues. It can be classified into several types:
Allergic Angioedema: Triggered by allergens like foods, insect bites, or medications.
Hereditary Angioedema (HAE): A genetic condition caused by C1-inhibitor deficiency.
Acquired Angioedema: Often linked to autoimmune diseases or malignancies.
Drug-Induced Angioedema: Commonly associated with ACE inhibitors or NSAIDs.
Idiopathic Angioedema: When the cause is unknown.
Symptoms include swelling, pain, or warmth in the affected area, and in severe cases, difficulty breathing or swallowing. Identifying the type and trigger is critical for tailoring treatment.
Acute Treatment Options
For acute angioedema episodes, rapid intervention is essential to alleviate symptoms and prevent complications.
1. Antihistamines
Antihistamines are the first-line treatment for allergic angioedema. They block histamine, reducing swelling and itching. Over-the-counter options like cetirizine or diphenhydramine are effective for mild cases, while prescription antihistamines may be needed for severe reactions. These medications work best when taken early in an episode.
2. Corticosteroids
Oral or intravenous corticosteroids, such as prednisone or methylprednisolone, are used to reduce inflammation in moderate to severe allergic angioedema. They are typically prescribed for short-term use to avoid side effects like weight gain or immune suppression. Corticosteroids are less effective for hereditary or non-allergic angioedema.
3. Epinephrine
In life-threatening cases, such as angioedema affecting the throat or causing anaphylaxis, epinephrine is administered via auto-injector (e.g., EpiPen). It rapidly reduces swelling and opens airways. Patients with a history of severe allergic reactions should carry epinephrine at all times.
4. C1-Inhibitor Concentrates
For hereditary angioedema (HAE), C1-inhibitor concentrates (e.g., Berinert, Cinryze) are highly effective. These replace the deficient protein, halting the cascade that causes swelling. They are administered intravenously and are critical for acute HAE attacks. Plasma-derived or recombinant forms are available.
5. Bradykinin Receptor Antagonists
Icatibant (Firazyr) is a targeted therapy for HAE that blocks bradykinin, a peptide responsible for swelling. It is injected subcutaneously and provides rapid relief. It is particularly useful for patients who do not respond to antihistamines or corticosteroids.
6. Fresh Frozen Plasma
In emergencies where C1-inhibitor concentrates are unavailable, fresh frozen plasma can provide C1-inhibitor and other proteins to stop HAE attacks. However, it carries risks like transfusion reactions and is less commonly used.
Preventive and Long-Term Treatments
For patients with recurrent or chronic angioedema, long-term management focuses on preventing episodes and addressing underlying causes.
1. Identifying and Avoiding Triggers
Patients should work with healthcare providers to identify triggers. Common culprits include certain foods (e.g., shellfish, nuts), medications (e.g., ACE inhibitors), or environmental factors. Avoiding these can significantly reduce episode frequency. For drug-induced angioedema, switching to alternative medications is often necessary.
2. Prophylactic Medications for HAE
For hereditary angioedema, prophylactic treatments reduce attack frequency:
C1-Inhibitor Therapy: Regular infusions of Cinryze or Haegarda prevent attacks by maintaining adequate C1-inhibitor levels.
Lanadelumab (Takhzyro): A monoclonal antibody that inhibits kallikrein, reducing bradykinin production. It is administered subcutaneously every two to four weeks.
Danazol: An androgen that increases C1-inhibitor production, though its use is limited by side effects like liver toxicity.
3. Immunosuppressants
In acquired or idiopathic angioedema, immunosuppressants like cyclosporine or methotrexate may be used to control underlying autoimmune processes. These are typically reserved for cases resistant to other treatments.
4. Antibiotics and Infection Management
Infections can trigger angioedema in some patients, particularly those with underlying immune deficiencies. Antibiotics like cephalexin, supplied by a cephalexin supplier, may be prescribed to treat bacterial infections that exacerbate swelling. Cephalexin is a first-generation cephalosporin effective against skin and soft tissue infections, which can indirectly reduce angioedema triggers. However, antibiotics are not a primary treatment for angioedema itself.
Lifestyle and Supportive Measures
In addition to medical treatments, lifestyle changes can help manage angioedema:
Stress Management: Stress can trigger episodes, particularly in HAE. Techniques like yoga, meditation, or counseling may help.
Dietary Adjustments: Avoiding known food allergens and maintaining a balanced diet supports overall health.
Medical Alert Bracelets: Patients with severe or hereditary angioedema should wear bracelets to inform emergency responders of their condition.
Regular Monitoring: Routine check-ups with an allergist or immunologist ensure treatment plans remain effective.
Special Considerations
Drug-Induced Angioedema
Angioedema caused by ACE inhibitors (e.g., lisinopril) or NSAIDs requires immediate discontinuation of the offending drug. Alternative medications, such as ARBs (e.g., losartan), may be prescribed. Symptoms may persist for weeks after stopping the drug, necessitating temporary use of antihistamines or corticosteroids.
Pediatric and Geriatric Patients
Children and older adults may require adjusted dosages or alternative treatments due to differences in metabolism or comorbidities. Pediatric HAE patients, for example, may use weight-based dosing for C1-inhibitor concentrates.
Pregnancy
Pregnant women with HAE require careful management, as some medications (e.g., danazol) are contraindicated. C1-inhibitor concentrates are generally safe and preferred during pregnancy.
Role of Cephalexin in Angioedema Management
While cephalexin, sourced from a Cephalexin supplier, is not a direct treatment for angioedema, it plays a supportive role in managing infections that may trigger or worsen episodes. For instance, bacterial skin infections or upper respiratory infections can exacerbate swelling in susceptible individuals. Cephalexin is typically prescribed for 7–10 days, depending on the infection’s severity. Patients should complete the full course to prevent resistance and monitor for side effects like allergic reactions, which could paradoxically trigger angioedema in rare cases.
Emerging Treatments
Research into angioedema continues to yield promising therapies:
Gene Therapy: Experimental treatments aim to correct C1-inhibitor deficiencies in HAE.
Oral Kallikrein Inhibitors: Drugs like berotralstat (Orladeyo) offer convenient alternatives to injectables for HAE prophylaxis.
Biologics: New monoclonal antibodies targeting pathways involved in angioedema are under investigation.
Conclusion
The best treatments for angioedema depend on its type, severity, and triggers. Acute episodes are managed with antihistamines, corticosteroids, epinephrine, or HAE-specific therapies like C1-inhibitor concentrates or icatibant. Long-term management involves trigger avoidance, prophylactic medications, and lifestyle adjustments. Antibiotics like cephalexin, supplied by a Cephalexin supplier, may support treatment by addressing infections that exacerbate symptoms. Patients should collaborate with healthcare providers to develop personalized plans, ensuring rapid symptom relief and prevention of future episodes. Advances in targeted therapies continue to improve outcomes, offering hope for better management of this challenging condition.